For a high level overview of Remote Monitoring - including Chronic Care Management (CCM), Remote Therapeutic Monitoring (RTM) and Remote Physiological Monitoring (RPM) - see “About Remote Monitoring”. For in-depth guidance on launching or revitalizing an RPM program, visit our “Remote Physiological Monitoring Toolkit”.
Medicare Billing for RPM Services
The Centers for Medicare and Medicaid Services (CMS) updates RPM CPT billing codes and reimbursement rates annually to support the continued adoption of remote monitoring and care management services. The sections below summarize 2025 Medicare billing guidance for RPM, including average national reimbursement rates and key program requirements.
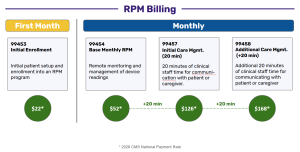
RPM services are billed using a set of CPT codes that correspond to different components of care, including device setup, data transmission, and ongoing clinical management , Billing differs in the first month of a patient's participation compared to subsequent months, depending on the level of clinical time and engagement required.
RPM services are billed using a series of CPT codes, which represent specific stages and levels of patient care. The image below illustrates how billing works in both the first month of a patient’s participation and in subsequent months, depending on the time and effort required from clinical staff.
In the first month, providers bill CPT 99453, which covers the initial patient setup and enrollment into the RPM program. This includes helping the patient understand how to use their monitoring device and getting their data connected to the clinic’s system. The reimbursement for this one-time setup activity is $20.
After the first month, billing shifts to a monthly structure to reflect ongoing care and monitoring:
CPT 99454 represents the base monthly RPM service, which involves the clinic reviewing and managing the patient’s remote device readings. This foundational service is reimbursed at $43 per month.
CPT 99457 adds 20 minutes of care management time by clinical staff who communicate directly with the patient or caregiver about their readings, progress, and care plan. When this level of support is provided, the total monthly reimbursement is $91.
For patients who require more intensive management, providers can add CPT 99458, which covers an additional 20 minutes of communication and coordination time. This raises the total monthly reimbursement to $129 for 40 minutes of clinical engagement.
Providers receive higher reimbursement when they spend more time actively managing a patient’s care, which encourages a more individualized and responsive approach.
CPT Codes for RPM Services
| Code | Description | Rate* |
| 99453 |
|
$21.71 |
| 99445 |
|
$52.11 |
| 99454 |
|
$52.11 |
| 99470 |
|
$26.05 |
| 99457 |
|
$51.77 |
| 99458 |
|
$41.42 |
* average national payment rate for this code in 2026
RPM Billing Requirements and Criteria
RPM services are classified as Evaluation and Management (E/M) services. CPT codes 99457 and 99458 may be furnished by a physician or other qualified health care professional, or by clinical staff under general supervision of a practitioner who is eligible to bill Medicare for E/M services.
To bill RPM services in 2025, the following requirements apply:
Patient and Clinical Requirements
- RPM may be used for both chronic and acute condition
- The patient must be an established patient (new patients require an initial evaluation prior to RPM enrollment)
- Patient consent must be obtained and documented before ordering RPM devices
- RPM services must involve active clinical monitoring and management, not passive data collection alone.
Device and Data Requirements
- RPM device must meet the FDA definition of a medical device
- Data collection and transmission must be HIPAA-compliant
- For CPT 99453 and 99454, at least 16 days of physiologic data must be collected within a 30-day period (Note: CMS has indicated this requirement is expected to be removed beginning Jan 2026)
Other Program Rules
- When multiple RPM devices are used, services may be billed only once per patient per 30-day period
- CPT 99453 may be billed only once per episode of care, defined as the period beginning with RPM initiation and ending when targeted treatment goals are met.
- Patients who were enrolled in RPM during the COVID-19 Public Health Emergency (PHE) may continue participation under current rules.
A Note on RPM Reimbursement for FQHCs & RHCs
Prior to 2024, RPM services were not separately reimbursable for Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs), limiting adoption despite demonstrated clinical value.
In January 2024, CMS introduced HCPCS code G0511 to allow FQHCs and RHCs to bill for chronic care management services, including RPM. However, this approach bundled multiple services into a single payment rate, creating confusion and making it difficult to accurately reflect the scope and intensity of RPM services delivered.
Beginning in January 2025, CMS revised its reimbursement policy to better align FQHC and RHC billing with Medicare fee-for-service standards. Instead of relying on the generalized G0511 code, FQHCs and RHCs may now bill RPM using the same CPT codes as other Medicare providers.
- 99453 – Initial setup and patient education
- 99454 – Device supply and data transmission
- 99457 – First 20 minutes of RPM care management
- 99458 – Each additional 20 minutes of care management
(See the CPT Codes for RPM Services table above for details.)
Why This Matters. This policy change allows FQHCs and RHCs to:
- Bill more accurately for services actually delivered
- Receive stronger financial support for RPM programs
- Expand access to RPM in rural and underserved communities
- Support long-term program sustainability and growth
Beginning in January 2026, RPM became more flexible with new codes (99445 and 99470) allowing reimbursement for as few as 2 - 15 days of data and 10 minutes of management time. Beyond these codes, Medicare also:
- implemented a 3.26% to 3.77% base reimbursement increase
- permanently authorized virtual direct supervision for teaching physicians via real-time audio-video
- introduced new Advanced Primary Care Management (APCM) add-on codes for behavioral health.
Additional Covered Care Management Services (2025)
Patients enrolled in Remote Physiological Monitoring (RPM) often have multiple chronic conditions and a history of high emergency department or hospital utilization. In addition to RPM, many of these patients benefit from other Medicare-covered care management services that support care coordination, patient engagement, and proactive intervention—helping to reduce avoidable, costly, and stressful events such as 911 calls or hospitalizations.
CMS allows several care management services to be billed alongside RPM, provided that the same clinical time and activities are not billed twice. Time spent delivering RPM services cannot be counted toward another care management service (such as Chronic Care Management).
Chronic Care Management (CCM)
Chronic Care Management (CCM) supports patients with two or more chronic conditions expected to last at least 12 months (or until death) and that place the patient at significant risk of:
- Death
- Acute exacerbation or decompensation
- Functional decline
CCM is a foundational primary care service that improves outcomes through structured, longitudinal care management.
Core CCM Service Elements
- Structured recording of patient health information
- Development and maintenance of a comprehensive electronic care plan
- Care coordination across settings and providers
- Management of care transitions
- Timely communication and sharing of patient information
These elements apply to both:
- Non-complex CCM (at least 30 minutes/month), and
- Complex CCM (at least 60 minutes/month),
unless otherwise specified by CMS.
Remote Therapeutic Monitoring (RTM)
Remote Therapeutic Monitoring (RTM) supports the management of patients using non-physiologic data, such as:
- Therapy adherence
- Therapy response
- Patient-reported outcomes
Unlike RPM—which focuses on objective physiologic measures (e.g., blood pressure, glucose, weight)—RTM captures subjective or self-reported data, commonly used for:
- Musculoskeletal conditions
- Respiratory conditions
- Behavioral health interventions
RTM services are typically furnished by qualified health care professionals, such as:
- Physical therapists
- Occupational therapists
- Speech-language pathologists
When used in combination with RPM, RTM can provide a more complete picture of patient progress, supporting personalized and coordinated care.
New Care Management Services
In addition to CCM and RTM, health professionals may bill for several care management services introduced or expanded by CMS:
- Behavioral Health Integration (BHI, 2018): Team-based, collaborative care integrating primary care and mental or behavioral health services.
- Principal Care Management (PCM, 2020): Management of a single high-risk chronic condition requiring frequent monitoring and treatment adjustment.
- Chronic Pain Management (CPM, 2023): A comprehensive, multidisciplinary approach for patients with pain lasting longer than three months, including structured assessment, monitoring, and care planning.
- Community Health Integration (CHI, 2024): Services that address social drivers of health (SDOH) that interfere with diagnosis or treatment, including care coordination and access facilitation.
- Principal Illness Navigation (PIN, 2024): Navigation services for patients with a serious, high-risk illness expected to last at least three months and associated with elevated risk of hospitalization, functional decline, or death.
- Advanced primary care management (APCM, 2025): A proactive, personalized approach to healthcare focused on continuous, holistic care with an emphasis on prevention, chronic disease management, and patient-provider communication (see below for more detail).
Advanced Primary Care Management (APCM) - New in 2025 | Expanded in 2026
Advanced Primary Care Management (APCM) is a Medicare service finalized in the 2025 Physician Fee Schedule, representing CMS’s most recent effort to support continuous, proactive, and holistic care for patients with chronic conditions.
APCM introduces a dedicated set of HCPCS codes with monthly bundled payments and integrates elements of several existing care management and communication technology–based services into a single, streamlined model.
APCM Allows Providers To:
- Deliver services tailored to patient complexity and care needs
- Emphasize prevention, chronic disease management, and care coordination
- Bill using a monthly bundled payment, rather than tracking and billing time minute-by-minute
Unlike traditional care management codes, APCM is not time-based. Providers may bill once per patient per calendar month after meeting required service elements and documentation criteria—significantly reducing administrative burden.
2026 APCM Updates: Behavioral Health Integration. In 2026, CMS expanded APCM to more seamlessly integrate behavioral health services, while further reducing administrative complexity. A major improvement is the introduction of new, non–time-based Behavioral Health Integration (BHI) add-on codes.
Unlike traditional BHI and CoCM CPT codes (e.g., 99484, 99492), which required detailed time tracking, these new HCPCS G-codes simplify documentation and are intended to encourage broader adoption.
New 2026 Behavioral Health APCM Add-On Codes
- HCPCS G0568 – Initial month of psychiatric Collaborative Care Model (CoCM) services
- HCPCS G0569 – Subsequent months of psychiatric CoCM services
- HCPCS G0570 – General Behavioral Health Integration (BHI) services
These add-on codes align with APCM’s bundled, non–time-based approach while expanding access to integrated behavioral health care.
Why APCM Matters
APCM enables practices to:
- Provide a wide range of services matched to patient complexity
- Reduce documentation burden compared to traditional care management models
- Shift focus from time tracking to care quality and continuity
Once all required elements are met, providers submit a single APCM HCPCS code per month, simplifying billing compared to traditional CCM, BHI, or CoCM services.
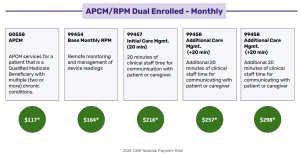
Example: RPM/APCM Dual Billing
Primary care providers—including FQHCs and RHCs—may pair RPM with APCM, as the services address different but complementary aspects of patient care.
- APCM supports continuous, interdisciplinary care coordination and population-based management
- RPM provides near–real-time physiologic data that enables early intervention and informed clinical decision-making
Because RPM time-based CPT codes were not included in CMS’s list of duplicative APCM services, qualified RPM clinical time may be billed separately, provided all billing and documentation requirements are met. Together, RPM and APCM support a data-informed, proactive chronic care model that improves patient outcomes while strengthening financial sustainability.
Sources:
- https://www.acponline.org/practice-career/business-resources/telehealth-guidance-and-resources/remote-patient-monitoring-billing-coding-and-regulations-information
- https://www.cms.gov/newsroom/fact-sheets/calendar-year-cy-2025-medicare-physician-fee-schedule-final-rule
- https://www.cms.gov/files/document/chroniccaremanagement.pdf
- https://www.cchpca.org/?policy=6503
- https://www.cms.gov/medicare/payment/fee-schedules/physician-fee-schedule/advanced-primary-care-management-services

