In today’s healthcare landscape, digital and remote care programs are transforming how patients are monitored and supported between in-person visits. Chronic Care Management (CCM), Remote Therapeutic Monitoring (RTM), and Remote Physiologic Monitoring (RPM) are three key approaches that enable clinicians to track patient health, intervene early, and coordinate care more effectively.
What is Chronic Care Management (CCM)?
Chronic Care Management (CCM) supports patients with two or more chronic conditions that require ongoing medical attention and care coordination. CCM includes developing and maintaining care plans, monitoring progress, and facilitating communication among healthcare providers. By providing structured, continuous support, CCM helps prevent complications, reduce hospitalizations, and improve overall patient health outcomes.
What is Remote Therapeutic Monitoring (RTM)?
Remote Therapeutic Monitoring (RTM) is a newer digital health service introduced by CMS to complement RPM. RTM focuses on monitoring non-physiologic data — such as therapy adherence, pain levels, functional status, or respiratory symptoms — typically for patients receiving therapeutic interventions like physical therapy or respiratory care. Data is collected using FDA-approved digital tools, apps, wearable sensors, or connected devices, and is reviewed by a clinical team to guide treatment decisions. RTM supports personalized therapy adjustments, improves patient outcomes, and enhances coordination between clinicians and patients.
What is Remote Physiological Monitoring (RPM)?
Remote Physiological Monitoring (RPM) is the periodic or continuous collection, transmission, and review of patients’ physiological data to inform care decisions. The physiological data collected depend on the patient’s diagnosis and may include weight, blood pressure, pulse, temperature, blood glucose, oximetry, respiratory flow rate, and heart rhythm.
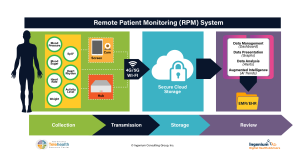
RPM uses FDA-approved digitally-enabled vital sign sensors such as a blood pressure cuff, a scale, continuous glucose monitoring (CGM), etc. to collect and then wirelessly transmit the data. The data is then presented to a clinical monitoring nurse or technician that periodically reviews the data, typically once a day.
When the patient’s vital signs are outside their established normal range, the care team can get in touch with the patient to confirm the measurements and, if needed, to work with the patient’s primary care provider (PCP) to improve the care plan (e.g., modifying their medication) to bring the patient back into a normal range.
This approach greatly minimizes the risk of undetected, unmanaged worsening of the patient’s health and can prevent unplanned urgent care, emergency care, or even hospitalizations.
What is RPM used for?
The two primary use cases for RPM are Readmission Prevention and Chronic Disease Management.
Readmission Prevention aims at keeping patients stable after a hospital discharge, by closely watching their vital signs and adjusting medication, nutrition, rehabilitation therapy and other care plan elements as needed. The financial case for Readmission Prevention lies in many health insurers not paying for a same-cause readmission within 30 days of discharge.
Chronic Disease Management uses RPM to stabilize patients’ conditions, especially in patients with 2 or more chronic diseases, including hypertension, COPD, congestive heart failure (CHF), diabetes, etc. The primary aim is to reduce avoidable utilization such as unplanned urgent care, or emergency care and hospitalizations, as well as the development of additional comorbidities.
In the following video Kathy Wibberly, director of the Mid-Atlantic Telehealth Resource Center, provides an overview of RPM.
What are some specific RPM use cases?
There are many use cases for RPM. Here are just a few examples:
- The American Heart Association has issued Using Remote Patient Monitoring Technologies for Better Cardiovascular Disease Outcomes
- The Personal Connected Health Alliance has put together this article on Understanding Remote Patient Monitoring in COPD
- The Rural Health Information Hub has this spotlight on Telehealth Invigorating and Innovating Diabetes Care
- mHealth Intelligence has published an article on Telehealth Gives Patients a Real-Time Link to Mental Health Support
- The California Health Care Foundation has published this paper on Remote Patient Monitoring in the Safety Net: What Payers and Providers Need to Know
- Telehealth Tuesday has published Dashboard Medicine: Remote Physiological Monitoring (RPM) driving Engagement & Outcomes
What kinds of devices can be used for RPM?
While many patients are monitoring their own health with consumer-grade devices embedded in smart watches or rings — such as activity trackers as well as heart rate, heart rhythm, heart rate variability and sleep monitors — clinical decision making requires that the devices are FDA approved.
- The US Food & Drug Administration (FDA) regulates medical devices sold in the United States to assure their safety and effectiveness. An RPM device is considered by the FDA as a wireless medical device.
- In response to the COVID-19 public health emergency (PHE), the FDA issued a new policies that allowed manufacturers of certain FDA-cleared non-invasive vial sign-measuring devices to expand their use so that health care providers can use them to monitor patients remotely. On March 24,2023, the FDA provided guidance related to the unwinding of the PHE. These may be found at:
What is the best way to start an RPM program?
Visit our Remote Physiological Monitoring Toolkit and our Remote Monitoring Billing and Reimbursement Guide!
The toolkit is designed to help provider organizations to get started. View the videos to understand roles and responsibilities and then make sure you download the actual RPM Toolkit - a PDF with lots of great information. When you are ready, explore our billing and reimbursement guide. Accurate billing and documentation are essential to ensure program sustainability and compliance.
Additional tools and resources:
- The California Telehealth Resource Center (CTRC) has:
- The Great Plains Telehealth Resource & Assistance Center (gpTRAC) Remote Physiological Monitoring Toolkit
- The US Department of Health & Human Services (Telehealth.HHS.gov) Telehealth and Remote Physiological Monitoring Overview
- Telehealth Tuesday has published a number of articles on selecting vendors, designing workflows, increasing ROI and preventing failure

