Outsourcing Clinical Telehealth Services
Key considerations for deciding whether to develop clinical telehealth services in house vs. working with outside vendors
Outsourcing is a great way to quickly scale existing expertise or to add additional expertise:

Overcome staffing shortages

Overcome recruitment challenges - in rural and urban areas

Validation of the market's / patients' interest in the services before you invest in establishing the service in house
Examples of Telehealth Services outsourcing:
Recruiting Telepsychiatric providers for rural areas
Increasing bed census for rural hospitals through virtual access to critical care
Adding a TeleSpeech Therapist to your pediatric practice
Adding a TeleRheumatologist to your hospital or a TeleGenetic Counselor
Starting a remote physiological monitoring program with outsourced monitoring nursing staff (called remote patient monitoring or RPM)
When outsourcing clinical services, maintaining Continuity of Care is essential for ensuring high-quality clinical outcomes. A critical requirement is that all care encounters provided by outsourced clinicians are documented within a shared medical record to support seamless care coordination. Without proper documentation and integration, patient care may become fragmented.
Challenges of Outsourcing Telehealth Clinical Services
While outsourcing can provide access to specialized expertise and help address workforce shortages, it also comes with potential drawbacks, including:
- Limited Control Over the Patient Experience – External clinicians may not fully align with your organization's culture, protocols, or approach to care.
- Clinical Documentation & EHR Integration Issues – If outsourced providers don’t use your EHR or if there is no integration with their system, capturing and accessing clinical notes can be difficult.
- Challenges with Care Coordination & Handoffs – Ensuring proper communication between internal and external providers can be complex, leading to potential gaps in patient care.
- Provider Turnover & Staffing Stability – You may have little control over clinician retention on the vendor’s side, leading to inconsistent care and frequent turnover.
- Limited Supervision & Quality Assurance – Your organization may have minimal oversight of vendor-employed clinicians, making it harder to enforce quality and performance standards.
- Scalability Limitations – If demand increases, the vendor may not have the capacity to quickly scale up services.
- Ongoing Costs & Financial Risks – Outsourcing comes with recurring vendor fees, and pricing may increase over time.
- Potential Conflict with Internal Clinicians – In-house providers may feel resentment toward higher-paid virtual clinicians, leading to workplace tension.
- Reliance on Vendor Stability – Vendors can face financial instability, acquisitions, or leadership changes, impacting service continuity and long-term reliability.
- Policy & Procedure Changes Beyond Your Control – The vendor may update policies or service structures without your input, affecting your organization's operations.
When Does Outsourcing Make Sense?
Outsourcing telehealth clinical services can be a great solution when working with a trusted, proven partner. It can also serve as a stepping stone for organizations considering bringing a service in-house—allowing time to evaluate demand before committing to full-time clinician recruitment.
By carefully weighing the benefits and risks, your organization can determine whether outsourcing aligns with your strategic goals, patient care priorities, and operational needs.
Establishing the Relationship with a Clinical Telehealth Service Vendor
1
Define Your Strategic, Business & Clinical Case
Before searching for a vendor, gain clarity on your organization’s needs by developing three key cases:
- Strategic Case: How does this service align with your organization’s goals and telehealth strategy?
- Business Case: What are the costs, revenue model, ROI projections, and financial sustainability factors?
- Clinical Case: Will this service meet the desired standard of care and be accepted by your clinicians?
Additionally, create a list of selection criteria, clearly separating must-have requirements from preferences to guide your vendor search.
2
Research Potential Clinical Service Vendors
Questions to consider include:
- Service Model: Are they standalone/virtual only service provider or a service offering by health systems or academic medical centers?
- Leadership and Experience: What is the composition and experience of their leadership team?
- Financial Stability: Is the vendor venture capital (VC)-funded, privately owned, or a subsidiary? VC-backed startups often grow rapidly but may require large service minimums or fail if funding dries up.
- References and Client Feedback: Seek honest insights from current clients, but recognize that each organization’s culture and integration needs are unique.
- Hiring and Quality Standards: Understand the vendor’s clinician selection, training process, and quality assurance measures.
3
Select a Telehealth Clinical Service Vendor
- Compare Sample Contracts: Ask multiple vendors for sample contracts so you can see what is typically included in a telehealth services contract. The differences in contract detail is indicative of the vendor's thoughtfulness and sophistication.
- Minimize Risk: Structure agreements to avoid long-term commitments until the service has proven effective.
- Clarify Billing & Performance Metrics: Establish clear billing procedures, reporting requirements, and performance benchmarks.
4
Onboard Your Clinical Telehealth Service Vendor
- Security and Compliance: Ensure that the vendor's policies match your organization's policies. e.g., HIPAA.
- Credentialing, Liability, Confidentiality, etc.: Create clarity around the credentialing with your organization, liability insurance, non-disclosure agreements.
- Fee Structure: Obtain a comprehensive fee schedule and fee guarantee timeframe.
- Privacy Policy: Read in detail all contracts and pay attention to the privacy policy to see if the vendor plans to share your patient's data with partners or outside companies.
- Patient/Patient Data Ownership: Clarify who owns the patient and the patient's data, the vendor or your organization?
- Patient Consent: All of these policies have to be consented to by your patients. What is the appropriate policy and procedure?
- Clinical Documentation: Ideally you would provide the vendor's clinicians access to your EHR or, at a minimum, ensure that the clinical notes are also made available in your EHR if the service provider requires their clinician to document the encounters in their own EHR.
- Welcome the Clinicians: In a peer-to-peer communication, e.g, from your chief medical officer, welcome the vendor's clinicians and share with them your organization's approach to patient care and what you feel are the unique characteristics of your patient population or even your region.
5
Develop and Validate Service Workflows
- Referral process: How will you refer patients to the outsourced service? Policies around the referral process also include service level agreements around the time to respond, time to care. Make sure that your staff understands the process on the vendor's side and What communication back to your team can be expected.
- Scheduling: How will you schedule patients and clinicians?
- Onboarding (new patients): How will you handle new patients differently than established patients?
- Rooming: How will the virtual visit be started? Are patients coming into your clinic to virtually connect to the virtual provider? Are patients at home? Is there someone from your staff or the service's'' vendor's staff that first meets the patient? Is there a copay collection before, during, or after the visit?
- Visit & clinical documentation & billing documentation: What Is the proper protocol by which you want the virtual clinician to provide the care, as defined by your clinical leadership? How does the visit need to be documented in your EHR for clinical and billing purposes?
- Post-visit & follow-up: What happens right after the virtual visit? Will someone from your organization follow up with the patient? What communication Is the service's vendor responsible for? What happens in the following days, weeks? Is there standard communication?
- Billing: What documentation is required for billing (see "visit" above)? Who is collecting the co-pay (see "rooming" above)? Who's billing whom (see "contract negotiations" above)? What other financial payments between your organization and the vendor are triggered by a patient visit in either direction?
A best practice for testing and validating all those workflows ("trust, but verify") is to have the vendor run you through their patient experience as a "mock patient".
For more information on the workflows involved in the delivery of care at a distance see the article "Telehealth and the 7 Thworfs". While that article focuses primarily on in-house provided video visits, the principles still apply.
6
Deploy New Workflows and Ensure Adoption
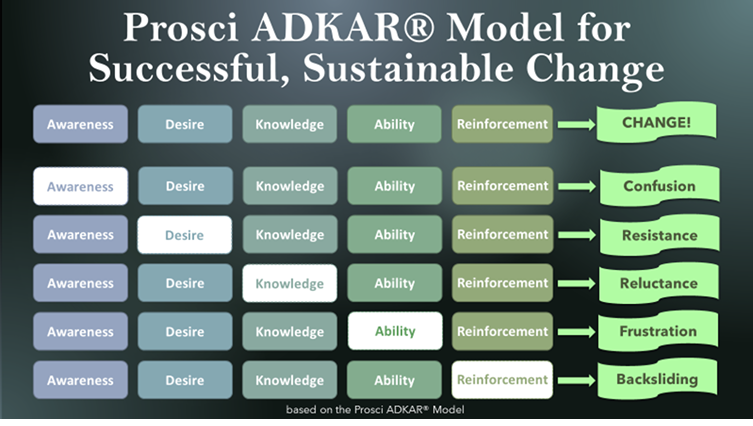
- Change Management: Understanding the integration of a new telehealth service as an exercise in change management is the first step toward success. Change is oftentimes uncomfortable to some and scary to others. One proven change management model is the ADKAR model for successful, sustainable change. For more information see the article "Telehealth Success through Conscious Change Management".
- Training: Workflow deployment mostly happens through the review of the workflows (if the users were not involved in the design of the new processes). This can include the review of the various happy day scenarios (what will happen 80%, 90% of the time) and the alternate scenarios (things that are expected to happen and how to react. Training mostly focuses on providing the Knowledge and the Ability for users to follow the new process. For more information see the article "A Proven Recipe for Telehealth Workflows".
- Support: The successful rollout of a new process depends on the availability of support if things do not go as planned.
- Accountability: The final step in the ADKAR model requires the provision of accountability to ensure that the newly implemented services are actually being used as intended to provide the promised or expected value.
![]() All
All
Sections
Section 1
Section 2
Section 3
Telehealth Technology Vendor Selection





